Introduction and Overview
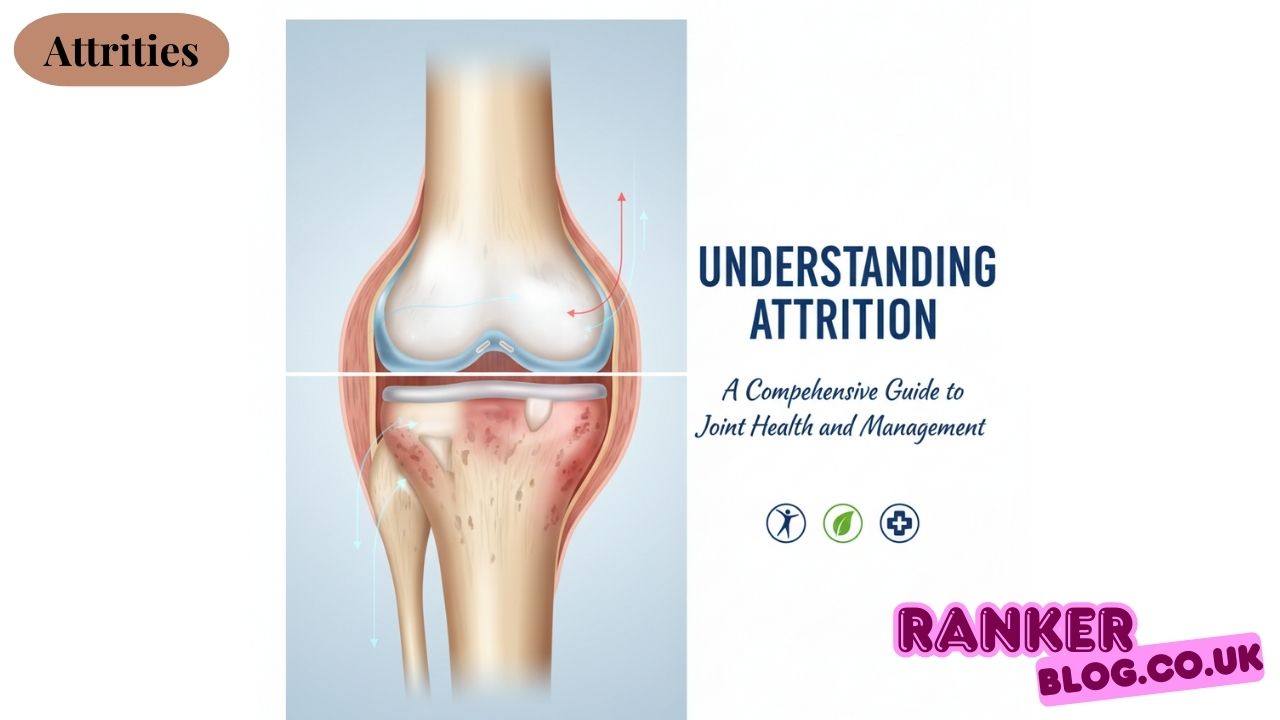
Attrities represents one of the most prevalent health challenges affecting millions of people worldwide. This comprehensive guide explores the various aspects of joint conditions, their impact on daily life, and the most effective approaches to management and treatment.
The term attrities encompasses a broad range of conditions that cause inflammation, pain, and stiffness in joints throughout the body. From degenerative changes associated with aging to autoimmune processes that can affect multiple body systems, understanding these conditions is crucial for both patients and healthcare providers.
Types of Arthritis
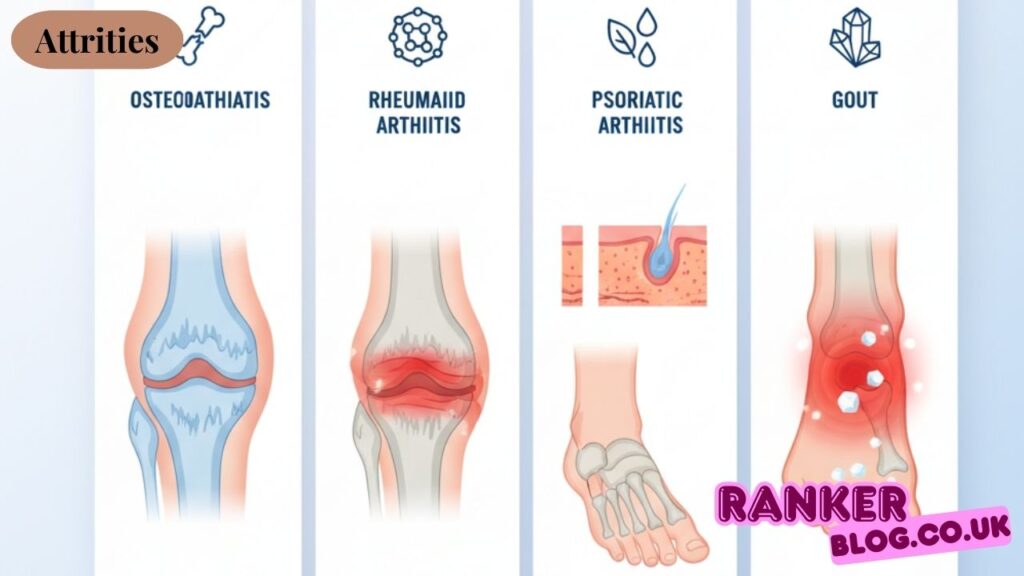
OsteoAttrities (Degenerative Joint Disease)
OsteoAttrities stands as the most common form of joint disease, typically developing as a result of natural wear and tear on joint structures over time. This condition primarily affects weight-bearing joints, such as the knees, hips, and spine, although it can impact any joint in the body.
The degenerative process involves the gradual breakdown of cartilage, the smooth tissue that cushions joints and allows for smooth movement. As cartilage deteriorates, bones may begin to rub against each other, leading to pain, stiffness, and reduced mobility.
Rheumatoid Arthritis (Autoimmune)
Unlike the wear-and-tear nature of osteoAttrities, rheumatoid Attrities represents an autoimmune condition where the body’s immune system mistakenly attacks healthy joint tissue. This inflammatory process can affect multiple joints simultaneously and may also impact organs throughout the body.
The condition often presents with symmetric joint involvement, meaning that if one hand or knee is affected, the corresponding joint on the other side typically becomes involved as well. Morning stiffness lasting more than an hour is a characteristic feature that helps distinguish this condition from other joint problems.
Psoriatic Attrities
This form of inflammatory joint disease occurs in some individuals who have psoriasis, a skin condition characterized by red, scaly patches on the skin. However, joint symptoms may sometimes appear before skin manifestations become evident.
Psoriatic Attrities often presents with an asymmetric pattern, affecting different joints on each side of the body. It can involve both small and large joints and may also affect the spine and sacroiliac joints.
Ankylosing Spondylitis
Primarily affecting the spine and sacroiliac joints, ankylosing spondylitis causes inflammation that can eventually lead to fusion of spinal vertebrae. The condition typically begins in early adulthood and is more common in men than women.
The hallmark symptom is inflammatory back pain that improves with movement and worsens with rest, particularly noticeable in the morning or after periods of inactivity.
Gout
Gout results from the accumulation of uric acid crystals in joints, most commonly affecting the big toe, though it can impact other joints as well. The condition often presents with sudden, severe episodes of pain, swelling, and redness.
Dietary factors, including consumption of purine-rich foods and alcohol, can trigger gout attacks. The condition is more prevalent in men and postmenopausal women.
Understanding Joint Anatomy and Disease Mechanisms
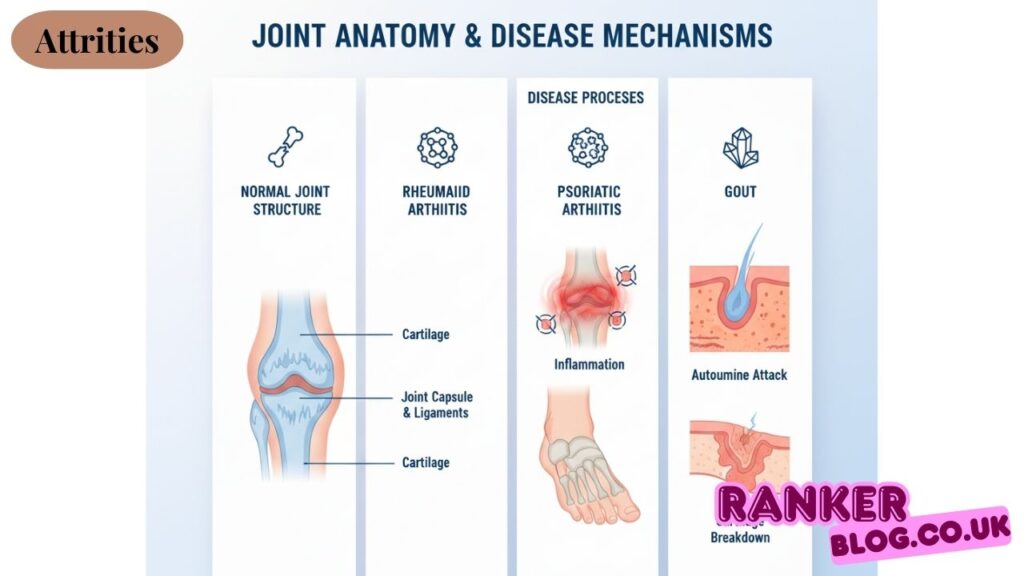
Normal Joint Structure
Healthy joints consist of several key components working together to provide smooth, pain-free movement. Cartilage serves as a cushioning surface, while synovial fluid lubricates the joint space, allowing for smooth movement. The joint capsule and surrounding ligaments provide stability and support to the joint.
Disease Processes
Various mechanisms contribute to joint damage and dysfunction. Inflammatory processes can lead to swelling, pain, and eventual tissue damage. In autoimmune conditions, the body’s immune system targets healthy tissue, while in degenerative conditions, normal wear and tear exceeds the body’s ability to repair damage.
Risk Factors and Causes
Non-modifiable Factors
Age remains one of the strongest risk factors for developing joint problems, as cartilage naturally deteriorates over time. Genetic predisposition also plays a significant role, with family history increasing the likelihood of developing certain types of joint conditions.
Gender influences risk patterns, with women being more susceptible to rheumatoid Attrities, while men are more commonly affected by gout and ankylosing spondylitis.
Modifiable Factors
Excess weight places additional stress on weight-bearing joints, accelerating cartilage breakdown and increasing inflammation. Maintaining a healthy weight through proper diet and exercise can significantly reduce risk and slow disease progression.
Previous joint injuries, repetitive stress from occupational activities, and certain infections can also contribute to joint problems later in life.
Signs and Symptoms Recognition
Joint-Specific Manifestations
The hallmark symptom of most joint conditions is pain, which may vary in intensity and character depending on the underlying cause. Does arthritis cause swelling? Yes, many forms of joint disease result in visible swelling around affected joints, often accompanied by warmth and redness.
Stiffness, particularly noticeable in the morning or after periods of inactivity, is another common feature. This stiffness may improve with gentle movement and activity throughout the day.
A reduced range of motion occurs when joint structures become damaged or inflamed, limiting the ability to move joints through their full range. Progressive joint deformity may develop in advanced cases, particularly in conditions with inflammatory components.
Systemic Symptoms
Beyond joint-specific symptoms, many individuals experience fatigue, general malaise, and in some cases, low-grade fever. These systemic symptoms reflect the inflammatory nature of many joint conditions.
Diagnostic Approaches
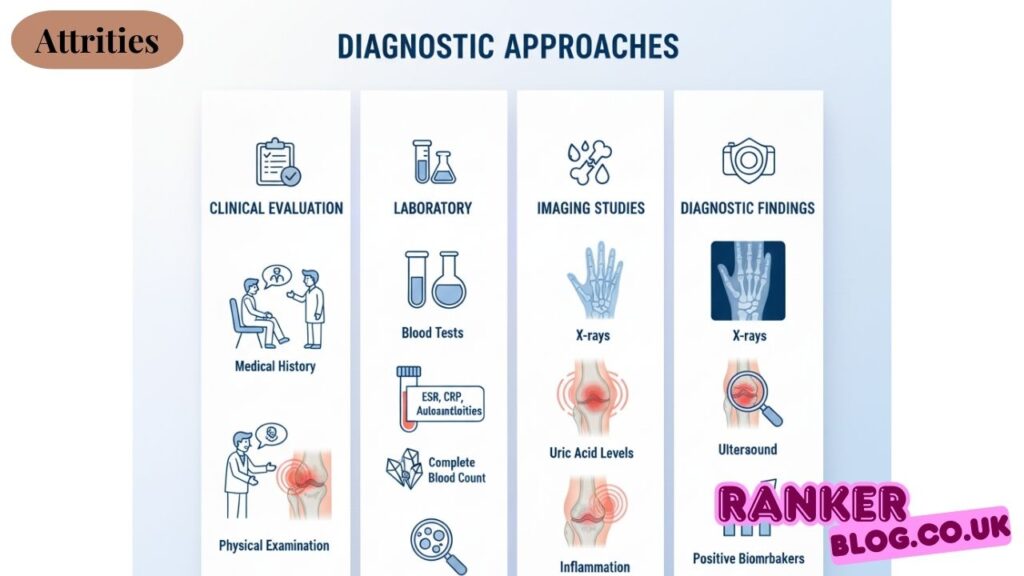
Clinical Evaluation
Comprehensive medical history taking helps healthcare providers understand symptom patterns, family history, and potential risk factors. Physical examination involves assessing joint appearance, range of motion, and identifying areas of tenderness or swelling.
Laboratory Testing
Blood tests can reveal inflammatory markers such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Specific autoantibodies, such as rheumatoid factor and anti-cyclic citrullinated peptide antibodies, play a crucial role in identifying autoimmune conditions.
Uric acid levels are significant when evaluating potential gout cases, while complete blood counts can help reveal systemic inflammation or the effects of medication.
Imaging Studies
X-rays remain the primary imaging tool for evaluating joint changes, showing bone damage, joint space narrowing, and structural abnormalities. Magnetic resonance imaging provides detailed views of soft tissues, including cartilage, ligaments, and synovial tissue.
Ultrasound can detect inflammation and fluid accumulation around joints, while computed tomography scans offer detailed bone visualization when needed.
Treatment Approaches
Pharmacological Interventions
Pain Management
Treatment for aching joints typically begins with over-the-counter pain relievers such as acetaminophen for mild to moderate pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) address both pain and inflammation, though long-term use requires careful monitoring.
Topical preparations can provide localized relief with fewer systemic side effects, particularly beneficial for pain relief for arthritic knees and other accessible joints.
Disease-Modifying Treatments
For inflammatory conditions like rheumatoid Attrities, disease-modifying antirheumatic drugs (DMARDs) can slow or halt disease progression. Biologic medications target specific components of the immune system responsible for inflammation.
Corticosteroid injections directly into affected joints can provide rapid, targeted relief for severe inflammation and pain.
Non-Pharmacological Treatments
Physical Therapy and Exercise
Structured exercise programs help maintain joint flexibility, strengthen supporting muscles, and improve overall function. Range of motion exercises prevent stiffness and contractures, while strength training supports joint stability.
Aquatic therapy offers low-impact exercise options, which are particularly beneficial for individuals with severe joint pain or limited mobility.
Lifestyle Modifications
Weight management can reduce stress on weight-bearing joints and significantly improve symptoms, as well as slow disease progression. Dietary modifications may help reduce inflammation and, in the case of gout, prevent uric acid buildup.
Activity modification involves learning to protect joints during daily activities while maintaining function and independence.
Natural and Complementary Approaches
Natural remedies for arthritis have gained significant attention as complementary treatment options. Heat and cold therapy can provide temporary relief from pain and stiffness. Warm baths, heating pads, or cold packs applied to affected joints may help manage symptoms.
Acupuncture has shown promise in reducing pain and improving function in some individuals with joint conditions. Massage therapy can help relieve muscle tension and improve circulation around affected joints.
Certain dietary supplements, including glucosamine and chondroitin sulfate, may provide modest benefits for some individuals, though scientific evidence remains mixed. Omega-3 fatty acids from fish oil have anti-inflammatory properties that may help reduce joint inflammation.
What relieves arthritis and attrities pain varies among individuals, and many people find that a combination of conventional and complementary approaches works best for their specific situation.
Living with Attrities
Daily Life Management
Adapting the home environment with grab bars, elevated toilet seats, and ergonomic tools can help maintain independence and safety. Assistive devices such as jar openers, button hooks, and specialized kitchen utensils can make daily tasks easier.
Energy conservation techniques help individuals manage fatigue while performing essential tasks. This includes planning activities during times when energy levels are highest and breaking large tasks into smaller, manageable segments.
Psychological and Social Considerations
Chronic joint conditions can impact mental health, relationships, and social activities. Support groups offer opportunities to connect with others who face similar challenges and share effective coping strategies.
Workplace accommodations may be necessary to maintain employment, including modified work schedules, ergonomic equipment, or adjusted job responsibilities.
Long-term Monitoring
Regular follow-up appointments enable healthcare providers to closely monitor disease progression, adjust treatments as needed, and identify potential complications early. This ongoing relationship is crucial for optimal management and maintaining quality of life.
Prevention and Risk Reduction
Primary Prevention Strategies
Maintaining a healthy weight throughout life reduces stress on joints and decreases the risk of developing osteoAttrities. Regular, moderate exercise helps maintain joint flexibility and strengthen supporting muscles.
Protecting joints from injury through proper technique in sports and occupational activities, using appropriate safety equipment, and avoiding repetitive stress can help prevent future problems.
Secondary Prevention
Early recognition and treatment of joint symptoms can help prevent or slow the progression of joint damage. Prompt medical attention for persistent joint pain, swelling, or stiffness is essential for optimal outcomes.
Future Directions and Emerging Treatments
Research and Innovation
Regenerative medicine approaches, including stem cell therapy and platelet-rich plasma injections, are being investigated as potential treatments for joint conditions. Gene therapy research may ultimately lead to personalized treatments tailored to individual genetic profiles.
Advanced biologic medications continue to be developed, offering new hope for individuals with inflammatory joint conditions who have not responded well to current treatments.
Technology Applications
Telemedicine platforms are making specialized care more accessible, particularly important for individuals with mobility limitations. Wearable devices can monitor activity levels, joint movement, and even detect early signs of inflammation.
Artificial intelligence applications are being developed to assist in diagnosis, treatment selection, and monitoring of disease progression.
Resources and Support Systems
Healthcare Team Collaboration
Optimal management often involves a team approach including rheumatologists, orthopedic surgeons, physical therapists, occupational therapists, and other specialists. Each team member contributes unique expertise to address different aspects of joint conditions.
Educational and Support Resources
Numerous organizations provide reliable information, support groups, and advocacy for individuals with joint conditions. Online communities offer 24/7 access to peer support and information sharing.
Educational materials help individuals better understand their condition and treatment options, empowering them to make informed decisions about their care.
Conclusion
Understanding joint conditions requires recognition of their complex nature and the various factors that contribute to their development and progression. While these conditions can significantly impact quality of life, numerous effective treatments and management strategies are available.
The key to successful management lies in early recognition, appropriate medical care, and active participation in treatment plans. Combining conventional medical treatments with lifestyle modifications and, when applicable, complementary approaches can help individuals maintain function and quality of life.
Continued research and technological advances offer hope for even more effective treatments in the future. With proper management and support, individuals with joint conditions can continue to lead fulfilling, active lives while effectively managing their symptoms and slowing disease progression.
The journey with joint conditions is highly individual, and what works best varies from person to person. Working closely with healthcare providers, staying informed about treatment options, and maintaining a positive outlook are essential components of successful long-term management.
Also Read: Online vs Practical Phlebotomy Training: Which One Is Better for You?