For many people experiencing chronic muscle pain, fatigue, and an invisible burden of discomfort that defies explanation, inomyalgia may be the term they’ve never heard but should know. Though still emerging in medical dialogue, inomyalgia refers to a class of conditions marked by persistent muscular pain, tenderness, and systemic fatigue, distinct from but related to fibromyalgia. This article offers a comprehensive, evidence-informed examination of what inomyalgia is, how it manifests, why it remains poorly understood, and what emerging research says about treatment and management. If you’re seeking answers for chronic pain that conventional diagnostics fail to explain, inomyalgia might be a key part of the puzzle.
What Is Inomyalgia?
Inomyalgia represents a complex chronic pain condition characterised by widespread muscle tenderness, persistent fatigue, and a constellation of symptoms that significantly impact daily functioning. Unlike many well-established medical conditions, inomyalgia exists in a relatively grey area of medical understanding, where researchers and clinicians are still working to define its precise boundaries and mechanisms.
The condition typically manifests as deep, aching muscle pain that persists for months or years, often accompanied by profound fatigue that doesn’t improve with rest. Patients frequently describe their experience as feeling as if their muscles are constantly inflamed or as if they’ve completed an intense workout, even when they haven’t engaged in physical activity.
Medical professionals who encounter inomyalgia often note its similarity to fibromyalgia, yet patients frequently report distinct differences in pain patterns, triggers, and responses to treatment. This has led researchers to investigate whether inomyalgia represents a separate condition or perhaps a variant of existing chronic pain disorders.
Key Features and Symptoms
The symptom profile of inomyalgia encompasses both physical and cognitive manifestations that can vary significantly between individuals. Understanding these symptoms helps both patients and healthcare providers recognise potential cases and develop appropriate management strategies.
Primary Physical Symptoms:
- Deep, persistent muscle aching that affects multiple body regions
- Muscle stiffness, particularly pronounced in the morning
- Tender points throughout the body, similar to but distinct from fibromyalgia trigger points
- Chronic fatigue that doesn’t respond to adequate sleep
- Sleep disturbances, including difficulty falling asleep and non-restorative sleep
Secondary Manifestations:
- Cognitive difficulties, often described as “brain fog”
- Heightened sensitivity to touch, sound, or light
- Temperature regulation problems
- Digestive issues and gastrointestinal discomfort
- Mood changes, including increased irritability or emotional sensitivity
Variable Symptoms: Many individuals with inomyalgia report that their symptoms fluctuate in intensity, sometimes following predictable patterns related to weather changes, stress levels, or activity patterns. This variability can make the condition particularly challenging to manage and understand.
Causes and Risk Factors

Research into the underlying causes of inomyalgia remains ongoing, but several potential mechanisms have emerged from clinical observations and preliminary studies. Understanding these factors can help individuals and healthcare providers develop more targeted approaches to managing their conditions.
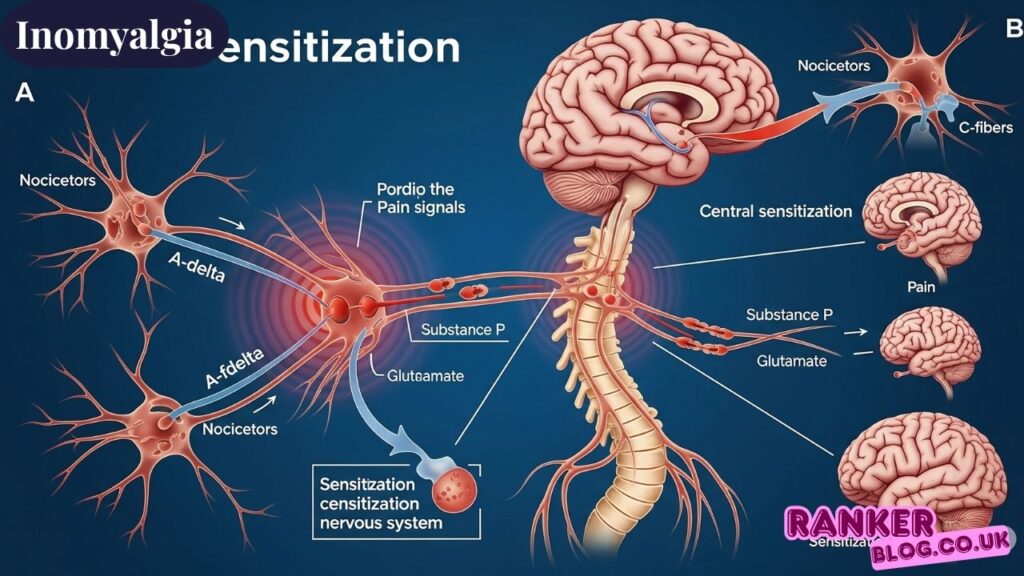
1. Central Sensitisation
Central sensitisation appears to play a crucial role in inomyalgia development. This process involves changes in how the central nervous system processes pain signals, resulting in amplified pain responses to normally non-painful stimuli. The nervous system essentially becomes hypersensitive, interpreting minor muscle tension or regular sensory input as significant pain signals.
2. Mitochondrial Dysfunction
Emerging research suggests that cellular energy production problems may contribute to inomyalgia symptoms. When mitochondria—the cellular powerhouses—function suboptimally, muscles may struggle to generate adequate energy for normal function, leading to persistent fatigue and pain.
3. Neurochemical Imbalances
Imbalances in neurotransmitters like serotonin, dopamine, and norepinephrine may influence pain perception and mood regulation in inomyalgia patients. These chemical messengers play crucial roles in how the body processes pain signals and maintains emotional balance.
4. Hormonal Fluctuations
Hormonal changes, particularly involving cortisol, thyroid hormones, and sex hormones, may trigger or exacerbate inomyalgia symptoms. Many patients report symptom changes that correlate with hormonal transitions such as menopause, pregnancy, or periods of high stress.
5. Genetic Predisposition
Family history studies suggest a possible genetic component to inomyalgia susceptibility. While specific genes haven’t been definitively identified, familial clustering of chronic pain conditions supports a hereditary influence.
6. Post-Infectious or Post-Trauma Onset
Some individuals develop inomyalgia following significant physical trauma, surgical procedures, or severe infections. This pattern suggests that major physiological stressors may trigger the condition in individuals who are susceptible.
How Inomyalgia Differs From Fibromyalgia
While inomyalgia and fibromyalgia share many characteristics, clinical observations reveal several distinguishing features that may help differentiate these conditions.
Pain Distribution Patterns: Inomyalgia pain often follows more anatomically specific patterns, frequently affecting particular muscle groups or regions asymmetrically. Fibromyalgia typically presents with more widespread, symmetric pain distribution.
Trigger Point Characteristics: The tender points in myofascial pain syndrome (inomyalgia) may differ in location and sensitivity patterns compared to the standardised fibromyalgia tender points. Patients often report that inomyalgia trigger points feel deeper and more muscular rather than surface-level.
Response to Treatment: Many patients notice different responses to standard fibromyalgia treatments when dealing with inomyalgia. This observation has prompted researchers to investigate whether distinct therapeutic approaches might be more effective for inomyalgia specifically.
Symptom Onset and Progression: Inomyalgia may have different onset patterns, sometimes developing more gradually or following different trigger events compared to typical fibromyalgia presentations.
Diagnosis: Why It’s Complicated
Diagnosing inomyalgia presents significant challenges due to the absence of definitive diagnostic tests and the condition’s similarity to other chronic pain disorders. Healthcare providers must rely on clinical observation, patient history, and the exclusion of different situations.
Diagnostic Approaches Often Include:
Comprehensive Medical History: Healthcare providers carefully document symptom patterns, onset circumstances, family history, and previous medical treatments to build a complete clinical picture.
Physical Examination: Detailed physical assessment focuses on identifying tender points, muscle tension patterns, and neurological function. Providers may use pressure point testing to map pain sensitivity.
Laboratory Testing: While no specific test confirms inomyalgia, blood work helps rule out other conditions such as autoimmune disorders, thyroid dysfunction, or vitamin deficiencies that might cause similar symptoms.
Imaging Studies: MRI or other imaging may be used to exclude structural problems that could account for symptoms, though these tests typically appear normal in inomyalgia patients.
Symptom Tracking: Patients may be asked to maintain detailed symptom diaries to help identify patterns and triggers that could inform diagnosis and treatment planning.
Treatment and Management Options
Effective inomyalgia management typically requires a multifaceted approach that addresses both symptoms and underlying contributing factors. The concept of “inomyalgia kai farmaka” (inomyalgia and medications) highlights the significant role that pharmaceutical interventions often play in conjunction with lifestyle modifications.
1. Lifestyle Recalibration
Sleep Hygiene
Establishing consistent sleep patterns forms the foundation of inomyalgia management. Patients benefit from creating an optimal sleep environment, maintaining regular bedtimes, and addressing sleep disorders that may exacerbate their symptoms.
Stress Modulation
Since stress significantly impacts inomyalgia symptoms, developing effective stress management techniques becomes crucial. This may include meditation practices, breathing exercises, or professional stress counseling.
2. Nutritional Support
Dietary modifications can significantly impact inomyalgia symptoms. Anti-inflammatory eating patterns, adequate protein intake for muscle health, and identifying food triggers that may exacerbate symptoms all contribute to overall management success.
Key Nutritional Strategies:
- Emphasising omega-3 fatty acids for their anti-inflammatory properties
- Ensuring adequate magnesium and vitamin D levels
- Considering elimination diets to identify food sensitivities
- Maintaining stable blood sugar levels throughout the day
3. Physical Therapy and Movement
Gentle, progressive exercise programs help maintain muscle function while avoiding overexertion that might trigger symptom flares. Physical therapists experienced with chronic pain conditions can design individualised programs.
Effective Movement Approaches:
- Low-impact aerobic exercises like swimming or walking
- Flexibility and stretching routines
- Strength training with careful progression
- Mind-body practices such as yoga or tai chi
4. Medications and Supplements
The “inomyalgia kai farmaka” approach often includes various pharmaceutical and supplement options tailored to individual symptom patterns and treatment responses.
Commonly Prescribed Medications:
- Low-dose antidepressants for pain modulation and sleep improvement
- Anticonvulsants that can help with nerve-related pain
- Muscle relaxants for severe muscle tension
- Sleep medications when natural sleep improvements prove insufficient
Supplement Considerations:
- Magnesium for muscle function and relaxation
- Vitamin D for overall muscle and bone health
- Coenzyme Q10 for potential mitochondrial support
- Omega-3 supplements for anti-inflammatory effects
5. Psychological and Social Interventions
Chronic pain conditions, such as inomyalgia, significantly impact mental health and social functioning. Addressing these aspects becomes essential for comprehensive care.
Therapeutic Approaches:
- Cognitive-behavioural therapy to develop coping strategies
- Support groups connecting patients with similar experiences
- Family education to improve understanding and support
- Mindfulness-based stress reduction techniques
Inomyalgia and Work-Life Balance
Managing inomyalgia while maintaining professional responsibilities requires careful planning and often workplace accommodations. Many patients successfully continue working by implementing strategic modifications to their work environment and schedules.
Workplace Strategies:
- Flexible scheduling to accommodate symptom fluctuations
- Ergonomic improvements to reduce physical stress
- Regular breaks to prevent symptom escalation
- Clear communication with supervisors about accommodation needs
Career Considerations: Some individuals find that career changes become necessary to better accommodate their inomyalgia symptoms. This might involve transitioning to less physically demanding roles or exploring remote work opportunities.
The Future of Inomyalgia Research
Research into inomyalgia continues to evolve, with several promising areas of investigation that may lead to improved understanding and treatment options.
Biomarker Discovery
Scientists are working to identify specific biological markers that could help diagnose inomyalgia more definitively and track treatment responses objectively.
Mitochondrial Health Therapies
Given the potential role of cellular energy dysfunction in inomyalgia, researchers are exploring treatments that specifically target mitochondrial health and function.
Wearable Tech and AI Tracking
Advanced monitoring technologies may help patients and providers better understand symptom patterns and treatment responses in real-time.
Integrative Care Models
Healthcare systems are developing more comprehensive approaches that combine conventional medical care with complementary therapies for optimal inomyalgia management.
Living Well with Inomyalgia
Despite the challenges that inomyalgia presents, many individuals develop effective strategies for maintaining quality of life and pursuing meaningful activities.
Key Success Factors:
- Developing realistic expectations and goals
- Building strong support networks
- Maintaining open communication with healthcare providers
- Celebrating minor improvements and accomplishments
- Staying informed about new research and treatment options
Daily Management Techniques: Successful inomyalgia management often involves developing personalised daily routines that balance activity with rest, incorporate symptom-monitoring practices, and maintain flexibility for symptom fluctuations.
Final Reflection
Inomyalgia represents a complex chronic pain condition that requires patience, persistence, and often creativity in developing effective management strategies. While the medical understanding of this condition continues to evolve, patients and healthcare providers working together can develop practical approaches to managing symptoms and improving quality of life.
The journey with inomyalgia is highly individual, and what works well for one person may not be equally effective for another. This reality emphasises the importance of personalised treatment approaches and the ongoing need for research into this challenging condition.
For those living with inomyalgia, remember that seeking support, staying informed about treatment options, including “inomyalgia kai farmaka” approaches, and maintaining hope for continued improvements in understanding and treatment remain essential aspects of the journey toward better health and well-being.
FAQs
1. What exactly is inomyalgia, and how is it different from fibromyalgia?
Inomyalgia is a chronic pain condition characterised by persistent muscle pain, tenderness, and fatigue. While similar to fibromyalgia, inomyalgia often presents with different pain distribution patterns, distinct trigger point locations, and may respond differently to standard fibromyalgia treatments. The exact relationship between these conditions is still being researched.
2. What causes inomyalgia, and who is most at risk?
The exact cause of inomyalgia remains unclear, but researchers believe multiple factors contribute, including central sensitisation, mitochondrial dysfunction, neurochemical imbalances, and genetic predisposition. Risk factors may include a family history of chronic pain, previous trauma or infections, hormonal changes, and high stress levels.
3. How is inomyalgia diagnosed if there is no standard test for it?
Inomyalgia diagnosis relies on clinical evaluation, including comprehensive medical history, physical examination, and exclusion of other conditions. Healthcare providers assess symptom patterns, conduct tender point examinations, and may order tests to rule out other disorders. Symptom tracking over time often helps confirm the diagnosis.
4. What are the best treatment options for managing inomyalgia?
Effective inomyalgia management typically involves a comprehensive approach combining lifestyle modifications, physical therapy, medications, and psychological support. The “inomyalgia kai farmaka” concept emphasises that medication often plays a vital role alongside other treatments. Success usually comes from personalised treatment plans developed with healthcare providers.
5. Can people with inomyalgia live everyday lives and work full-time?
Many people with inomyalgia successfully maintain fulfilling lives and careers, though this often requires strategic planning and accommodations. Success factors include developing effective symptom management strategies, working with understanding employers on workplace modifications, and building strong support networks. While challenges exist, many patients find ways to pursue meaningful activities and professional goals.
Also Read: Asbestlint: Understanding Hidden Industrial Hazards and Safety Measures

